Jay Scannelly's Email & Phone Number
Corporate Vice President at HCA
Jay Scannelly Email Addresses
Jay Scannelly Phone Numbers
Jay Scannelly's Work Experience

Regional Vice President- Payer Contracting & Alignment- American & National Groups
January 2013 to Present


Regional Vice President- Payer Contracting & Alignment- American & National Groups
January 2013 to May 2022

Carolinas Healthcare System
Assistant Vice President
January 2011 to January 2013

Director, Strategic Pricing & Analytics- Capital and TriStar Divisons
January 2001 to January 2011


Director, Contracts and Development, Health Advantage Plans, Inc.
January 1997 to January 2001

Administrative Director – Transplant Center
January 1995 to January 1997
Show more
Show less
Frequently Asked Questions about Jay Scannelly
What is Jay Scannelly email address?
Email Jay Scannelly at [email protected], [email protected] and [email protected]. This email is the most updated Jay Scannelly's email found in 2024.
How to contact Jay Scannelly?
To contact Jay Scannelly send an email to [email protected], [email protected] or [email protected].
What company does Jay Scannelly work for?
Jay Scannelly works for HCA
What is Jay Scannelly's role at HCA?
Jay Scannelly is Director, Strategic Pricing & Analytics- Capital and TriStar Divisons
What is Jay Scannelly's Phone Number?
Jay Scannelly's phone (901) ***-*360
What industry does Jay Scannelly work in?
Jay Scannelly works in the Hospital & Health Care industry.
Jay Scannelly's Professional Skills Radar Chart
Based on our findings, Jay Scannelly is ...
What's on Jay Scannelly's mind?
Based on our findings, Jay Scannelly is ...
Jay Scannelly's Estimated Salary Range
Jay Scannelly Email Addresses
Jay Scannelly Phone Numbers
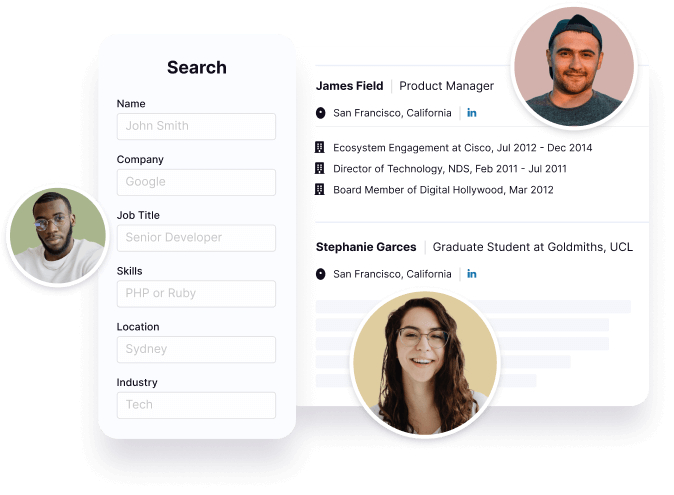
Find emails and phone numbers for 300M professionals.
Search by name, job titles, seniority, skills, location, company name, industry, company size, revenue, and other 20+ data points to reach the right people you need. Get triple-verified contact details in one-click.In a nutshell
Jay Scannelly's Ranking
Ranked #153 out of 3,052 for Director, Strategic Pricing & Analytics- Capital and TriStar Divisons in Tennessee
Jay Scannelly's Personality Type
Extraversion (E), Sensing (S), Feeling (F), Judging (J)
Average Tenure
2 year(s), 0 month(s)
Jay Scannelly's Willingness to Change Jobs
Unlikely
Likely
Open to opportunity?
There's 77% chance that Jay Scannelly is seeking for new opportunities
Top Searched People
American comedian and actress
American actress
American actor
American actress
Actor ‧ Todd Chrisley's daughter































Jay Scannelly's Social Media Links
/in/jay-scannelly-644b144 /company/hca /school/uab/ /redir/redirect