Farid Hassanpour's Email & Phone Number
Healthcare Executive, Innovative forward thinking Leader, Healthcare Consultant
Farid Hassanpour Email Addresses
Farid Hassanpour's Work Experience

EHS+C
Principal Consultant
January 2022 to Present



Health Net and California Health & Wellness / Centene
Chief Medical Director
July 2015 to November 2019

WellPoint
Medical Director
August 2013 to July 2015


CHOC Health Alliance / Aetna
Chief Medical Officer
January 2010 to June 2012


Inland Empire Health Plan
Associate Medical Director
January 2005 to January 2007

Santarus, Inc.
Scientific Affairs Liaison
October 2004 to October 2005

Bristol Park Medical Group
Director / Staff Physician
November 1996 to November 2004

UC Irvine The Paul Merage School of Business
MBA
January 2001 to January 2003

Miller Children's Hospital Long Beach
Pediatric resident
January 1992 to January 1995
Show more
Show less
Farid Hassanpour's Education
University of California, Irvine - The Paul Merage School of Business
January 2001 to January 2003
Des Moines University
January 1988 to January 1992
Show more
Show less
Frequently Asked Questions about Farid Hassanpour
What is Farid Hassanpour email address?
Email Farid Hassanpour at [email protected], [email protected] and [email protected]. This email is the most updated Farid Hassanpour's email found in 2024.
How to contact Farid Hassanpour?
To contact Farid Hassanpour send an email to [email protected], [email protected] or [email protected].
What company does Farid Hassanpour work for?
Farid Hassanpour works for EHS+C
What is Farid Hassanpour's role at EHS+C?
Farid Hassanpour is Principal Consultant
What is Farid Hassanpour's Phone Number?
Farid Hassanpour's phone (**) *** *** 386
What industry does Farid Hassanpour work in?
Farid Hassanpour works in the Insurance industry.
Farid Hassanpour's Professional Skills Radar Chart
Based on our findings, Farid Hassanpour is ...
What's on Farid Hassanpour's mind?
Based on our findings, Farid Hassanpour is ...
Farid Hassanpour's Estimated Salary Range
Farid Hassanpour Email Addresses
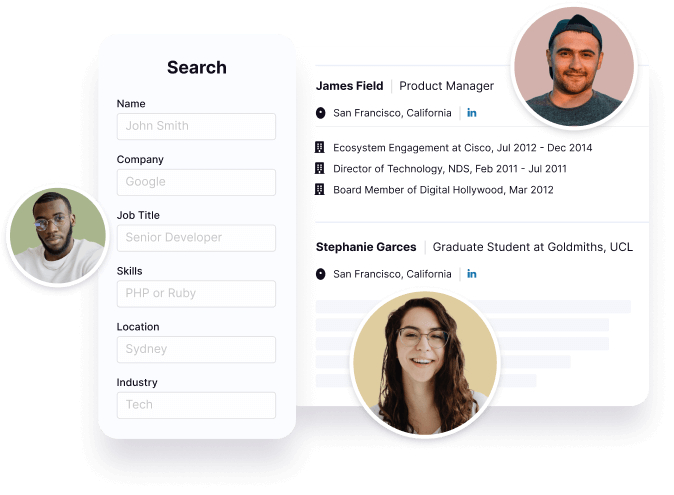
Find emails and phone numbers for 300M professionals.
Search by name, job titles, seniority, skills, location, company name, industry, company size, revenue, and other 20+ data points to reach the right people you need. Get triple-verified contact details in one-click.In a nutshell
Farid Hassanpour's Personality Type
Extraversion (E), Sensing (S), Feeling (F), Judging (J)
Average Tenure
2 year(s), 0 month(s)
Farid Hassanpour's Willingness to Change Jobs
Unlikely
Likely
Open to opportunity?
There's 87% chance that Farid Hassanpour is seeking for new opportunities
Top Searched People
Dutch Violinist and conductor
Chairperson of Leeds United
German former tennis player
Colombian model and actress
Mexican actress


























Farid Hassanpour's Social Media Links
/in/faridhassanpour cahealthwellness.com