Bernardo Costa's Email & Phone Number
Digital Transformation | Innovation | Business | M&A | Seed Investor
Bernardo Costa Email Addresses
Bernardo Costa Phone Numbers
Bernardo Costa's Work Experience

AgroVen
CoFounder and Chief Innovation Officer
June 2019 to Present

AgroVen
Founder
June 2019 to Present



Grupo Algar
Corporate and M&A Legal Counsel (Executive Lawyer)
November 2011 to December 2014


Grupo Algar
Senior Legal Counsel
September 2006 to November 2011



Escola de Idiomas Wisdom
English Teacher
January 2001 to December 2005


AgroVen
Show more
Show less
Bernardo Costa's Education
Insper
January 2016 to January 2018
Fordham University
January 2013 to January 2013
Fordham University
January 2013 to January 2013
Fundação Getulio Vargas
January 2011 to January 2012
IBET – Instituto Brasileiro de Estudos Tributários
January 2007 to January 2008
Show more
Show less
Frequently Asked Questions about Bernardo Costa
What is Bernardo Costa email address?
Email Bernardo Costa at [email protected] and [email protected]. This email is the most updated Bernardo Costa's email found in 2024.
How to contact Bernardo Costa?
To contact Bernardo Costa send an email to [email protected] or [email protected].
What company does Bernardo Costa work for?
Bernardo Costa works for AgroVen
What is Bernardo Costa's role at AgroVen?
Bernardo Costa is CoFounder and Chief Innovation Officer
What is Bernardo Costa's Phone Number?
Bernardo Costa's phone (**) *** *** 957
What industry does Bernardo Costa work in?
Bernardo Costa works in the Information Technology & Services industry.
Bernardo Costa Email Addresses
Bernardo Costa Phone Numbers
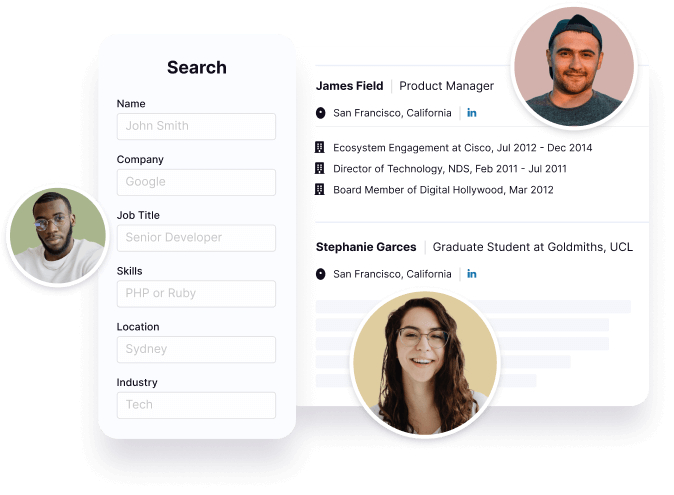
Find emails and phone numbers for 300M professionals.
Search by name, job titles, seniority, skills, location, company name, industry, company size, revenue, and other 20+ data points to reach the right people you need. Get triple-verified contact details in one-click.In a nutshell
Bernardo Costa's Personality Type
Extraversion (E), Intuition (N), Feeling (F), Judging (J)
Average Tenure
2 year(s), 0 month(s)
Bernardo Costa's Willingness to Change Jobs
Unlikely
Likely
Open to opportunity?
There's 71% chance that Bernardo Costa is seeking for new opportunities

























Bernardo Costa's Social Media Links
/in/bernardo-costa-7563b232